Much in the way I got into home birth, I think I am going to get into home death.
In other words, I feel like I am going to get pretty annoying, interpersonally, about how I want birth and death to be different in this country.
I say this by way of an apology/content warning. If you don’t want me to unload A Lot of Opinions about death over dinner, avoid the subject with me at all costs. I have A Lot of Opinions (what’s new).
For the past five or six years, I’ve developed a subgenre interest in reading a good deal about death and the elderly. Watching my beloved grandparents die and watching my parents care for them has certainly motivated this curiosity.
I have a layperson’s fascination with the culture of medicine and am grateful to count many excellent physicians and nurses among my close friends. They are incredibly impressive to me, and I have neither the intelligence nor emotional strength to do what they do. I’m fascinated by their work and how our culture is inextricably bound up in how we practice medicine and how we approach the end of our lives.
The more I’ve learned, the more I’ve found the following beliefs of the American monoculture on the old and dying to be extremely troubling.
1. We don’t want to talk—or even think—about death.
Dissertations and books have been written about this subject, so I’ll be brief, but I think the problems all start here.
In a nation that prizes the pursuit of happiness and prosperity above all else, death is incredibly repellent to us. We’ll do almost anything to avoid thinking about it.
Death is kept as far away from us as possible. We collect the dying in hospitals and nursing homes, far from our actual homes. We avoid any whiff of unpleasantness and death and shift it to those in the medical profession. We lie to our children about what happens to pets and grandparents when they die. We use a crazy array of euphemisms to describe death and the dying. We prefer to pretend it’s not happening (and that it will never, ever happen to us).
For most of human history, death was a very present, normal part of existence. We died with more regularity and from any number of causes. A mere 100 years ago in the U.S., for instance, 30% of babies and children died before the age of 5, compared with 1.5% today. Many people died from what we would today consider commonplace injuries and infections. I’m not saying this was great; God bless modern medicine! But death was everywhere.
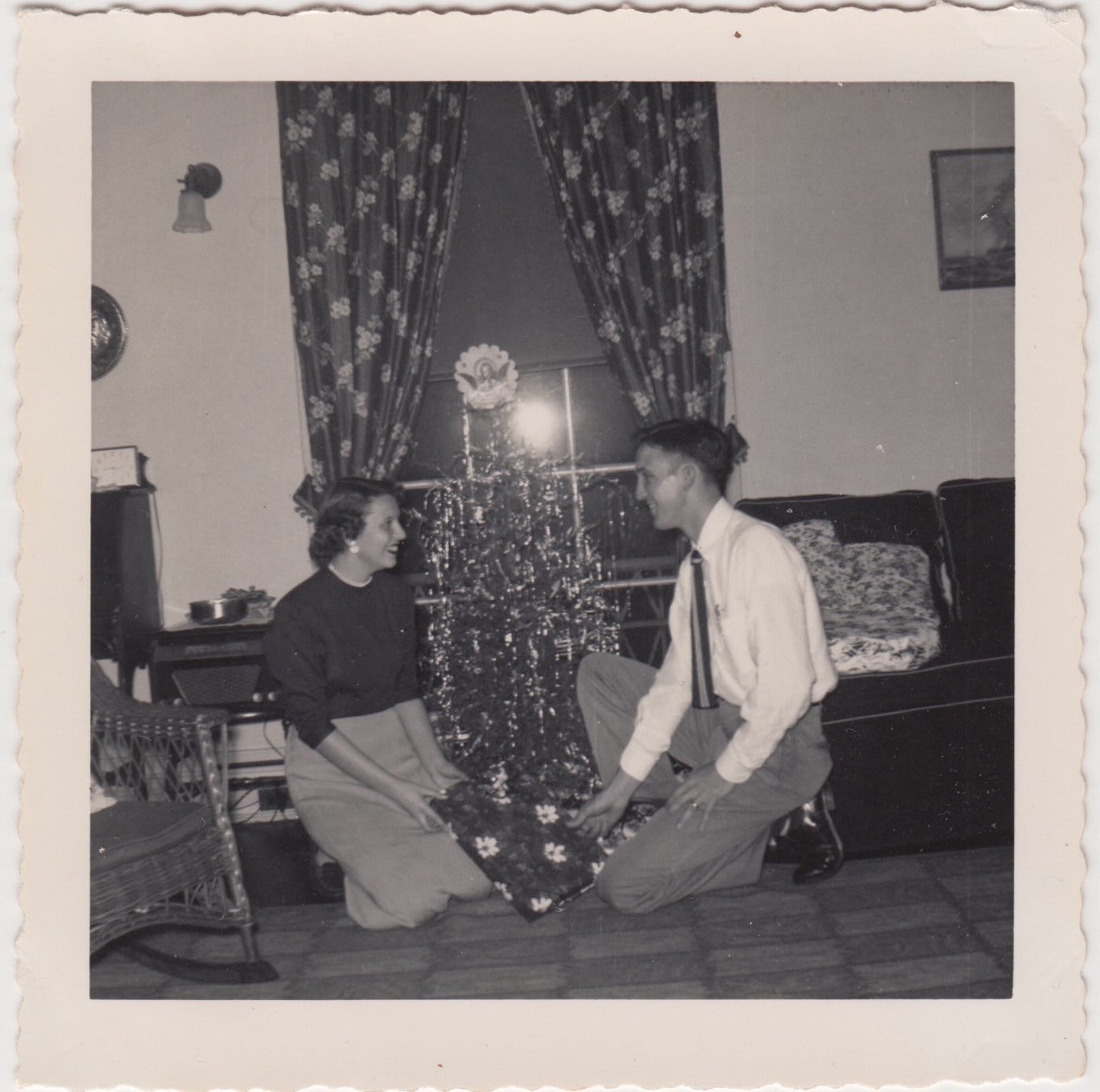
Parents and grandparents would be dying openly in the bed in the family room. Bodies would be literally decomposing on our kitchen tables as they were washed for the grave. Children and parents were witnessing each other’s deaths all the time. It was neither weird nor unusual, even as it was, of course, still deeply sorrowful.
“A culture that denies death is a barrier to achieving a good death.”
— Caitlin Doughty, Smoke Gets in Your Eyes
I’m not saying that I want to go back to this era, but I think we are paying for our ignorance and avoidance of death in some significant ways.
2. We don’t value the elderly.
Old people remind us of death, and as mentioned, we’d rather not think about that.
They’re slow and inconvenient, and we’d prefer to orient our lives toward the young, beautiful, and fit—and thus endeavor to see ourselves in those categories for as long as possible. The old are regarded as if they carry some form of contagion; if we talk about and to them too much, we’ll catch their mortality and may become old ourselves.
Many other cultures still value the elderly. We’re just not one of them. I was struck by this while reading Japanese folk tales to Moses recently. All of the heroes of Japanese folk tales are old people: obāchan and ojīchan (grandmother and grandfather). The stories revolve around their wisdom and clever ingenuity. We have no such similar stories here in America. In Disney, which is what we have instead, old people typically take the form of evil crones (usually women) who are trying to literally suck the life and youth out of the young heroes.
We discard and denigrate the elderly. They have no function in American society, except to be expensive burdens on the medical system. They are not regarded as elders. They are not regarded as precious. They are not protected. They are not, it seems, worthy of our attention and respect.
3. We prioritize quantity of life over quality of life.
A further consequence of our inability to reckon with mortality is that we try to prolong life as long as possible—even if it’s miserable.
We beg doctors to keep us and our loved ones alive at all costs, and even if we’re not begging, we’re frequently being told by physicians that there’s always one more thing we could try. Treat every disease with more drugs. Fix every possible ailment. Try another surgery. Separate this limb or organ from the rest of the failing system and treat it as an isolated part (instead of viewing the body and spirit as an inseparable whole).
“A body, love insists, is neither a spirit nor a machine; it is not a picture, a diagram, a chart, a graph, an anatomy; it is not an explanation; it is not a law. It is precisely and uniquely what it is. It belongs to the world of love, which is a world of living creatures, natural orders and cycles, many small, fragile lights in the dark.”
— Wendell Berry, “Health Is Membership”
Quality of life for the elderly often means helping them live independently and creatively. An onslaught of complicated, contraindicated medications and debilitating surgeries may extend life, sure, but keep an older person confined to bed or to a small room for years until they finally expire. Instead, we ought to be proactive about finding ways to live with disability and avoid interventions.
The medical system is organized to fix first, care second. But are we prolonging life? Or simply prolonging dying?
4. Nobody wants to die this way. But most of us do.
All four of my grandparents had complicated, drawn-out deaths, languishing in nursing homes for months and even years before they died.
They deserved better. I don’t want those deaths for my parents or for myself. I don’t think anyone does. And yet it’s how it usually goes.
In my reading, a striking pattern I’ve observed is that physicians often choose to do much less for themselves/their families than they do for their patients when it comes to end-of-life decisions. They have first-hand experience of how a cascade of medical interventions can make life much, much worse, not better, for the elderly. When pressed, health care professionals typically reject most medical interventions: no chemo past a certain age, no hip replacements, no resuscitations.
As a layperson, I’m very mindful of this finding. The health care system has evolved to make life last as long as possible, at any cost, and yet the practitioners in the system know that this often makes for a dreadful, prolonged end.
“In the twentieth century, American medicine became more interested in cosmetics and catastrophes than in promoting and preserving human health and well-being. In the twenty-first century, it worships machines, genes, neurons, hearts, and tumors, but cares little about sanity, walking, eating, frailty, or suffering. It values adults over the young and old, and hospitals and intensive care units over homes and clinics. It prioritizes treatment over prevention, parts over wholes, fixing over caring, averages over individuals, and the new over the proven.”
— Louise Aronson, Elderhood
What do I want to do differently?
Prioritize our elders. Help them. Listen to them. Find out what they need. Talk to them and write them letters. Learn from them and value their wisdom. Value their dignity and personhood (especially for the many with dementia, who are often treated as subhuman).
Talk about death a lot. Normalize dying and death. It’s not creepy; it’s not gross; it’s not unhealthy.
Talk about end of life desires a lot, with my parents, with my husband, with anyone who should know.
Write an advanced directive and do all that legal stuff. Get your will sorted out. Talk about how you want your funeral to go. Be as clear as possible about your wishes, long before you get into a state of cognitive or other bodily impairment.
Find and see a geriatrician and help my parents find one when the time is right.
Do whatever I can in my life to avoid taking medications. The fewer drugs you’re on, the better. Especially when you get past the age of 60.
Be ready and willing to say no to medical interventions (both now, in my time of relative health, and especially later). Pursue alternative methods of treatment and healing.
Explore ways to live with disability and manage pain. I can’t find the source now, but I loved this sentiment from a disability advocate: Living with disability is a beautiful, challenging opportunity for creative thinking. Some of the most powerful, creative thinkers we have are people living every day with their disability.
Explore alternative options for death at home. Most people want to die at home, if given the choice, but this becomes increasingly rare for those in a heavily medicated state. How can we reclaim dying in a peaceful, non-institutional environment?
Explore alternative options for natural burials (e.g., eco-friendly cemeteries that allow bodies to decompose into the earth). Along with being a far better way to go into the ground, natural burials also tend to be less expensive (because you don’t have to pay for things like vaults or impermeable coffins). As an aside, it’s funny to me that we consider this (along with home birth/home death) “newfangled,” when it’s the way most human beings have been doing death and burial for thousands of years.
Aging is frightening, and contemplating our mortality makes most of us shiver. But the older I get, the more conscious I am that life is short. Death comes for all of us. We do ourselves (and our children, and the present generations) a disservice to pretend like it’s not.
Media vita in morte sumus. In the midst of life, we are in death.
Recommended reading
Books
Being Mortal: Medicine and What Matters in the End, Atul Gawande
Elderhood: Redefining Aging, Transforming Medicine, Reimagining Life, Louise Aronson
How We Die: Reflections on Life’s Final Chapter, Sherwin B. Nuland
Knocking on Heaven’s Door: A Path to a Better Way of Death, Katy Butler
Smoke Gets in Your Eyes: And Other Lessons from the Crematory, Caitlin Doughty
The Emperor of All Maladies: A Biography of Cancer, Siddhartha Mukherjee
On Vanishing: Mortality, Dementia, and What It Means to Disappear, Lynn Casteel Harper
On Being Ill, Virginia Woolf
Illness as Metaphor, Susan Sontag
Articles and Other Websites
Why I Hope to Die at 75. A compelling piece from oncologist Ezekiel Emmanuel on his desire to die at the “young” age of 75. (The Atlantic)
The Order of the Good Death. Caitlin Doughty’s attempt to create an ars moriendi movement for the modern age.
Talk to me about death, if you dare, but especially if you’re my parents. Let’s chat.




I preach often on the fact of death, the reality of resurrection, and the need to get things right with God and your neighbor now, not later.
In my pastoral experience, I am struck by how separated death has become from dying. Often, I am only called after the fact, by the funeral home, to say a few prayers over an urn. The entire moment is disconnected from anything communal.
I appreciate the things you've said here. I work as a geriatric nurse doing long term care and geriatric rehabilitation. I have witnessed first hand the horrors of how our country dishonors the elderly. They are the most marginalized and neglected population in America, locked away in the prisons of our modern medical system. "Prison," in my opinion, is actually an understatement. Our elderly, due to unsafe staffing ratios (often 30 patients to one nurse) and lack of compassion, are not even allowed to use the toilet or be washed when they want. They are not stimulated emotionally, mentally, or socially. In their confused state of aging, they are often asked, "Why did you do that?" or are yelled at for their mistakes. They often die alone, cold, and dirty with an "admission" ready in the hall to fill their bed and fill the coffers of our greedy American systems. Families have their own reasons for how they manage the care of the aging loved ones. Some of those are legitimate reasons related to their own disablities or life situations, and I can't judge those families. They are doing the best they can. But some of the reasons are just selfish, and honestly, I have begun to even understand those selfish reasons. My own parents and in-laws are aging. It is hard to think about rearranging my life for an indefinite amount of time to manage their ever growing needs. Despite my convictions that are similar to yours regarding aging and death, I also see that it's complicated. I hope my husband and I can rise to the challenge of caring for them with grace, compassion, and love, with patience and selflessness, but I am not going to assume that just because I have these convictions that it is going to be easy. I know our lives will be richer and their lives will end more gracefully, if we can work together to honor them the way that we are called to.